Revenue Cycle Management (RCM)
At PROQ RCM, we understand that the Revenue Cycle Management (RCM) billing cycle is a crucial element for the financial health and operational efficiency of healthcare providers. Our approach to RCM is designed to ensure that healthcare organizations are reimbursed accurately and in a timely manner, while also minimizing administrative burdens.
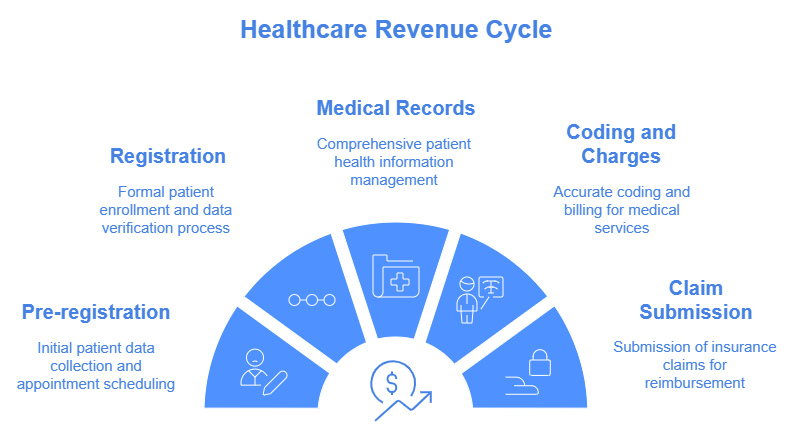
The RCM billing cycle is a series of steps that healthcare providers follow from the moment a patient makes an appointment, through to the collection of payments from insurers and patients. It involves multiple stages, including patient registration, insurance verification, medical coding, billing, claim submission, payment posting, and accounts receivable management. Each step is critical in ensuring that healthcare providers are paid for the services they deliver, and that financial and operational performance is optimized.
At PROQ RCM, we streamline this entire cycle by offering end-to-end billing solutions, leveraging technology, industry expertise, and a patient-centered approach to optimize each phase of the process. Whether it’s ensuring accurate claims submission, managing denials, or improving collections, we are committed to helping our clients achieve financial success and operational efficiency.
Explore our detailed services below to learn how we can support your practice’s revenue cycle from start to finish.
RCM Cycle Key Functions:
- Appointment scheduling management and Appointment reminders
- Insurance verification process (Eligiblity, Benefits & Obtaining Authorization)
- Medical Transcription & EMR maintainance
- Medical Coding
- Medical Billing
- Account Receivables & Denial Management
- Quality Management & Analytics
- Key Reports & proper utilization of AR Metrics in the RCM Process
- Provider credentialing & contracting / Enrollment process
- Types of training sessions to the providers & front office staff
- End-to-End RCM Technology and Vendor Integration for Comprehensive Workflow Management
Appointment scheduling management and Appointment reminders
- Appointment Scheduling Management is a critical part of the Revenue Cycle Management (RCM) process as it ensures efficient patient flow, reduces no-shows, and supports the billing and coding processes.
- Appointment reminders are crucial in minimizing no-shows and cancellations, which can lead to revenue loss and workflow disruptions.
Insurance verification process (Eligiblity, Benefits & Obtaining Authorization)
- Eligibility Verification - We confirm that patients' insurance coverage is active and valid at the time of service.
- Benefits Verification - We verify the patient’s benefits, including co-pays, deductibles, and coverage limits, ensuring clear financial expectations for both patients and providers.
- Obtaining Prior Authorization - For services requiring pre-approval, we secure the necessary authorizations, ensuring compliance with payer policies and reducing the chances of claim rejections.
Medical Transcription & EMR maintainance
- Medical Transcription, We provide accurate medical transcription services to convert physician voice files into detailed, organized text records that are essential for proper documentation and billing. Our transcription experts ensure that every patient interaction is precisely captured.
- Additionally, We offer comprehensive EMR (Electronic Medical Record) maintenance services, ensuring that patient records are consistently updated, organized, and accessible. This allows for seamless integration between clinical care and billing, improving workflow efficiency and ensuring that all documentation is accurate for coding and reimbursement purposes. Our solutions help healthcare providers maintain compliance, reduce errors, and enhance overall patient care management.
Medical Coding
- At PROQ RCM, our medical coding services ensure accurate translation of healthcare diagnoses, procedures, and treatments into standardized codes See more details
Medical Billing
- At PROQ RCM, Our comprehensive medical billing solutions are designed to optimize your revenue cycle. We handle complex claims, reduce administrative burdens, and accelerate payment processing, allowing you to focus on patient care See more details
Account Receivables & Denial Management
- At PROQ RCM, we specialize in Account Receivables (A/R) management to ensure timely payment collection and improve cash flow for healthcare providers. Our team tracks unpaid claims, follows up with insurance companies, and works to resolve payment issues efficiently.See more details
Provider credentialing & contracting / Enrollment process
- At PROQ RCM, We streamline the credentialing process to help providers join payer networks faster and maintain compliance with credentialing requirementsSee more details